Radionuclide synovectomy with 90yttrium (90Y)
A practical guide for referring physicians
Radionuclide synovectomy (RSO) is a minimally invasive therapeutic method used to treat chronic inflammatory changes in the synovium. The principle involves the intra-articular application of a β-emitter in the form of a colloidal suspension, whose ionising radiation causes controlled destruction of the hyperplastic synovial membrane.
90Y is a β-emitter with an energy of 2.3 MeV and a particle range of up to 11 mm, making it an ideal radioisotope for the treatment of large joints, especially the knee. It is used in the form of 90Y citrate or 90Y silicate colloid, which ensure localised retention in the joint cavity.
The effect of the therapy is gradual – over several weeks to months, effusions subside, pain is reduced and joint function improves.
Main clinical indications
- Rheumatoid arthritis of the knee – chronic synovitis unresponsive to systemic or local therapy.
- Psoriatic arthritis – persistent synovitis in the knee joint.
- Haemophilic arthropathy – recurrent haemarthrosis leading to synovial hypertrophy and secondary joint destruction.
- Degenerative gonarthrosis with reactive synovitis – when conservative treatment fails and TEP is postponed.
- Chronic non-specific synovitis, including after TEP – with repeated effusions and pain.
Contraindications
- Absolute: acute joint infection, severe joint destruction with instability.
- Relative: pregnancy, breastfeeding, generalised skin disease at the injection site, severe coagulation disorder, uncompensated systemic diseases.
Procedure
- Indications and preparation: determined by a rheumatologist or orthopaedic surgeon in consultation with a nuclear medicine physician. Infection must be ruled out (CRP, sedimentation, puncture if suspected). The patient must be informed and sign a consent form.
- Application:
- The procedure is performed under aseptic conditions.
- Puncture of the joint, evacuation of effusion.
- Intra-articular application of 90Y colloid (usual dose 185–250 MBq).
- Application of a small dose of corticosteroid to reduce the risk of reactive synovitis.
- Immobilisation: the knee is immobilised (elastic bandage, orthosis) for 48 hours to minimise RF leakage outside the joint.
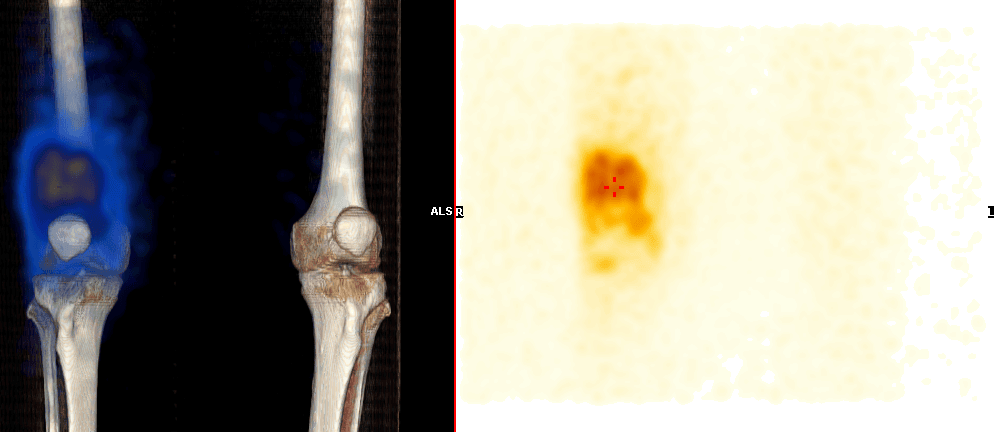
- Distribution control: post-injection scintigraphy to verify correct intra-articular application.
Efficacy and expected effect
- Onset of effect: within 4–12 weeks.
- Long-term effect: persists for 1–5 years, in some cases longer.
- Success rate: 60–80% of patients report improvement in pain, reduction in effusion and improvement in mobility.
- Best results: in early synovitis without severe degenerative changes.
Side effects and complications
- Local reactions: temporary pain, swelling in the first few days.
- Radiation synovitis: a rare complication with pain and swelling, usually transient.
- Extravasation of radiopharmaceutical: risk of radiation necrosis of the skin – prevention by proper technique and immobilisation.
- Infection: extremely rare when aseptic conditions are maintained.
Clinical examples
- Patient with rheumatoid arthritis of the knee – failure of DMARD and intra-articular corticosteroids, significant reduction in effusions after 90Y application, no pain after 6 months.
- Young haemophiliac with chronic haemarthrosis – after repeated bleeding, 90Y synovectomy performed, 80% reduction in haemarthrosis.
- Patient with grade III gonarthrosis – after 90Y RSO, pain relief and improved gait, indication for TEP postponed for several years.
Summary for practice
Yttrium-90 radionuclide synovectomy is:
- An effective and safe method for the treatment of chronic synovitis of large joints.
- A suitable alternative to surgical synovectomy in high-risk or polymorbid patients.
- A method with long-term effects that improves quality of life and reduces the need for invasive procedures.
- Optimally indicated for early and moderate forms of synovitis, especially of the knee joint.
When performed correctly, 90Y RSO is a proven therapeutic tool in nuclear medicine that combines effectiveness with minimal invasiveness and high clinical benefit.