Skeletal scintigraphy
A practical guide for referring physicians
Skeletal scintigraphy is one of the most commonly performed methods in nuclear medicine and is one of the basic tools for evaluating pathological changes in bone tissue.
After intravenous administration of a 99mTc-labelled diphosphonate radiopharmaceutical (most commonly HDP), it binds to the crystalline structure of hydroxyapatite in areas of increased bone turnover. This method visualises osteoblastic activity, which reflects ongoing tumour, traumatic, inflammatory or degenerative processes.
Whole-body planar scintigraphy is standard. In indicated cases, it is supplemented by:
- three-phase scintigraphy (perfusion, soft tissue and bone phases) – especially in cases of suspected osteomyelitis or fractures,
- SPECT/CT – fusion imaging providing detailed anatomical localisation and higher specificity.
The advantage is high sensitivity – changes in bone metabolism are detected within days, much earlier than morphological changes on X-ray or CT.
Main clinical indications
Oncology
- Detection of bone metastases – the most common indication (breast, prostate, lung, kidney and thyroid cancer).
- Staging and restaging of malignancies – rapid whole-body mapping of the extent of the disease.
- Evaluation of treatment response
- Differential diagnosis – SPECT/CT helps distinguish metastases from benign lesions (degenerative changes, fractures).
Traumatology and orthopaedics
- Occult and stress fractures invisible on X-ray.
- Tibial and femoral edge syndrome
- Distinguishing between old and new fractures.
- Assessment of bone graft viability and complications after osteosynthesis.
Infections and inflammations
- Osteomyelitis – typically positive in all three phases of scintigraphy.
- Diabetic foot – differentiation between bone infection and soft tissue involvement.
- Endoprosthesis complications – infection versus aseptic loosening.
Degenerative and rheumatological changes
- Arthrosis – typically increased activity in weight-bearing parts of joints.
- Rheumatoid arthritis – determination of activity and extent of involvement.
- Spondyloarthritis – distinguishing between active and resting phases.
Metabolic and other bone diseases
- Paget's disease – intense accumulation in affected areas.
- Avascular necrosis – characteristic "donut sign" (cold centre, hot rim).
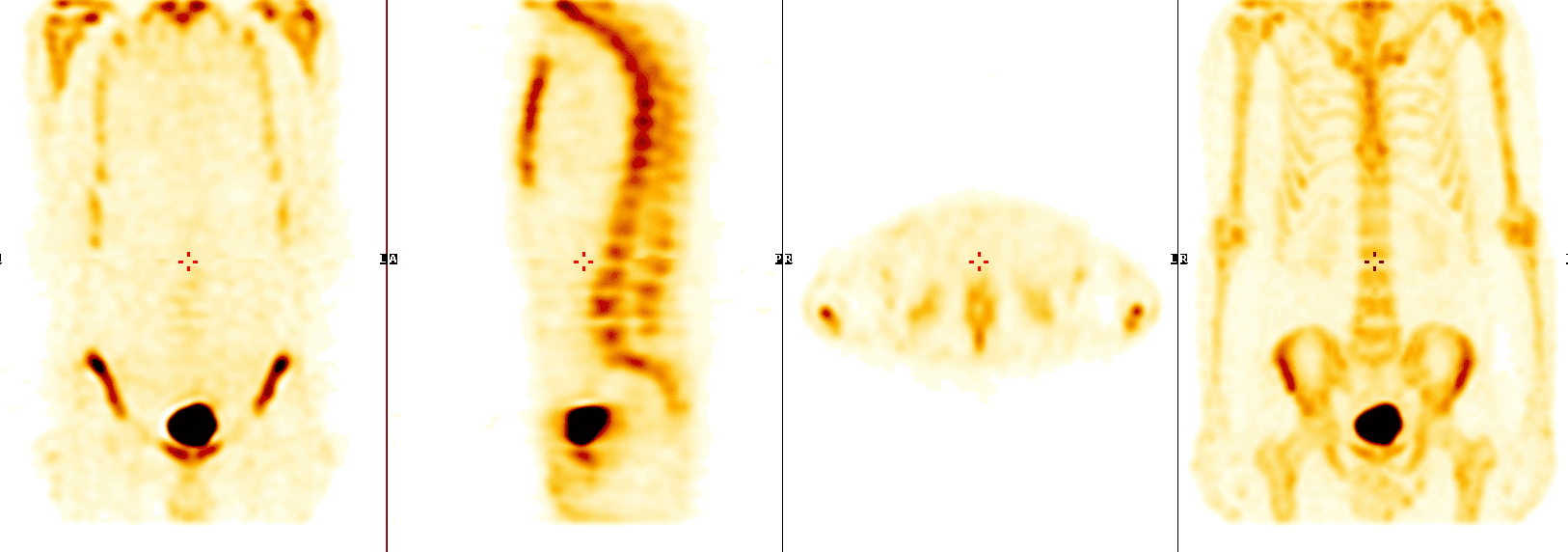
- Superscan – diffuse symmetrical uptake throughout the skeleton without renal excretion (e.g. diffuse metastases, severe metabolic disorders).
- Reflex sympathetic dystrophy (Sudeck's syndrome).
Interpretation
- High sensitivity – the method detects even small metabolic changes.
- Lower specificity – positive findings may also be caused by benign processes (degeneration, fractures, arthrosis).
- False negative findings: osteolytic lesions without osteoblastic reaction (e.g. multiple myeloma, renal carcinoma metastases).
- SPECT/CT significantly reduces the number of ambiguous findings, especially in the spine, pelvis and complex joints.
Interpretation must always be performed in the context of the clinical picture and other imaging methods (X-ray, CT, MRI, PET/CT).
Practical information for the referring physician
- Patient preparation: no special diet, hydration recommended.
- Duration of examination: administration of radiopharmaceutical, waiting for distribution (2–3 hours), then imaging (30–60 minutes). Total duration approx. 3–4 hours.
- Radiopharmaceuticals: 99mTc-HDP.
- Radiation exposure: 3–4 mSv (less than a whole-body CT scan).
- Contraindications: pregnancy; relative contraindication for breastfeeding women.
Clinical examples
- Patient with breast cancer – whole-body scintigraphy revealed multiple metastases in the spine and ribs that were not yet visible on X-ray.
- Young athlete – stress fracture of the tibia confirmed on scan, even though X-ray was negative.
- Patient after endoprosthesis implantation – SPECT/CT distinguished aseptic loosening of the stem from infection, which significantly influenced further treatment.
Summary for practice
Skeletal scintigraphy is:
- a basic method in oncology, orthopaedics, rheumatology and infectious medicine,
- a highly sensitive screening examination of the entire skeleton,
- valuable in the evaluation of metastases, fractures, osteomyelitis and metabolic bone diseases,
- an easily accessible and relatively inexpensive method with low radiation exposure.
Proper indication and supplementation with SPECT/CT significantly increase its informative value and make this method an indispensable tool in everyday clinical practice.