Perfusion scintigraphy of the myocardium under stress
A practical guide for referring physicians
Principle and method
Myocardial perfusion scintigraphy (myocardial perfusion SPECT, MPS) is a key nuclear medicine method for the non-invasive diagnosis of ischaemic heart disease (IHD), assessment of myocardial viability and risk stratification of patients.
The examination combines stress ergometry (physical stress on a bicycle ergometer or treadmill or pharmacological stress) with the administration of a perfusion radiopharmaceutical, which is taken up inside vital cardiomyocytes in proportion to coronary perfusion.
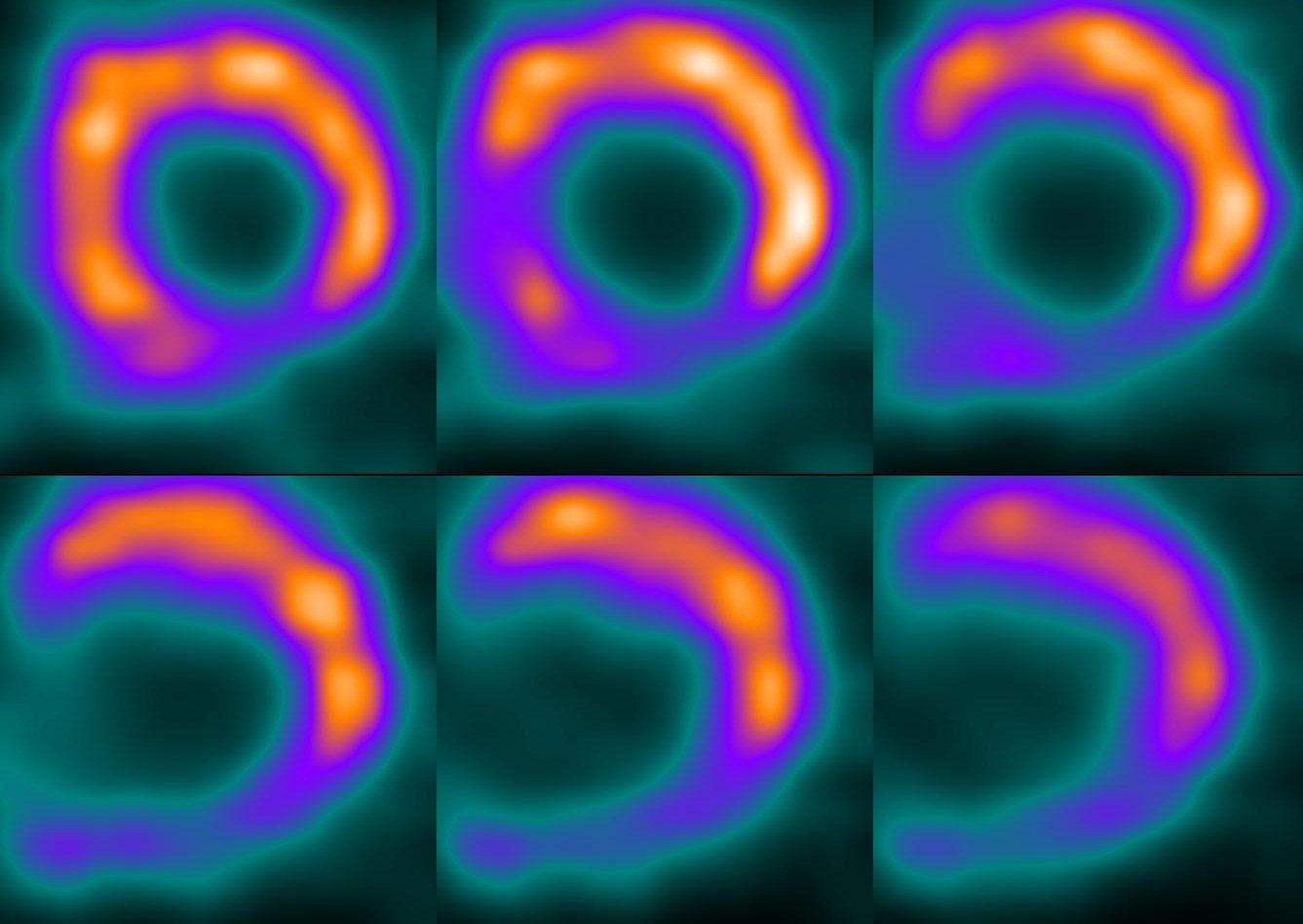
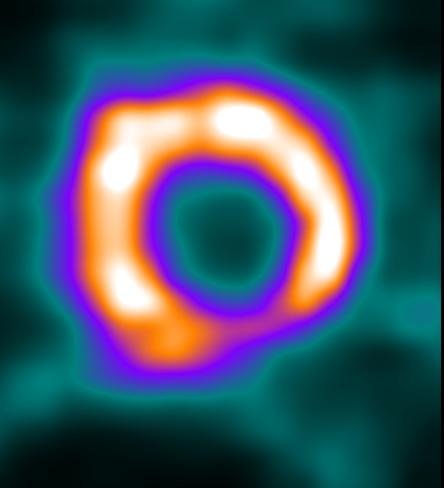
During exercise, coronary demands increase – the area supplied by a stenotic artery shows relative hypoperfusion, which appears as a defect on SPECT. By comparing images after exercise and at rest, reversible ischaemia can be distinguished from irreversible infarct damage.
Main clinical indications
1. Diagnosis of ischaemic heart disease
- Detection of ischaemic foci in patients with chest pain and suspected IHD.
- Assessment of the haemodynamic significance of coronary stenosis.
2. Prognostic stratification
- Determination of the risk of future cardiac events (heart attack, sudden death).
- The extent and severity of perfusion defects directly correlate with the patient's prognosis.
3. Indications for revascularisation
- Distinguishing between viable and non-viable myocardium.
- Deciding on the need for PCI or CABG.
4. Monitoring treatment efficacy
- After coronary interventions or bypass surgery.
- After pharmacological therapy for IHD.
5. Other indications
- Assessment of the causes of shortness of breath and unclear chest pain.
- Differential diagnosis between ischaemic and non-ischaemic cardiomyopathy.
Interpretation and clinical significance
Signs of stress ischaemia
- Reversible defect – perfusion disorder during exercise, normalising at rest → evidence of ischaemia.
- The location of the defect corresponds to the supply area of the affected coronary artery.
Signs of scarring
- Fixed defect – persistent hypoperfusion even at rest → irreversible myocardial necrosis.
Other indicators
- Quantification of defect extent (% of left ventricle).
- Evaluation of ejection fraction and wall kinetics (gated SPECT).
Practical information for the referring physician
- Patient preparation:
- fasting for 4–6 hours,
- discontinuation of beta-blockers or antianginal medication according to the cardiologist's instructions,
- avoid caffeine 24 hours before the examination.
- Examination procedure:
- the patient undergoes ergometry with graded exercise,
- upon reaching the target heart rate (85% of the maximum for the patient's age), a radiopharmaceutical is administered,
- distribution is followed by SPECT imaging,
- in the next step, a resting examination is performed for comparison.
- Examination duration: 3–4 hours.
- Radiation exposure: approx. 7–10 mSv.
- Contraindications: acute MI, unstable angina, severe arrhythmias, decompensated heart failure, severe aortic stenosis.
Summary for practice
Stress myocardial perfusion scintigraphy is:
- the gold standard for non-invasive diagnosis of ischaemic heart disease,
- a method with high sensitivity and specificity for detecting myocardial ischaemia,
- a tool for decision-making on revascularisation and prognostic stratification,
- a safe, accessible and clinically highly beneficial method.
Correct indication and interpretation significantly improve the diagnosis and treatment management of patients with IHD and remain an indispensable tool in modern cardiology.