Test for enterohepatic recirculation of bile acids – SeHCAT
A practical guide for referring physicians
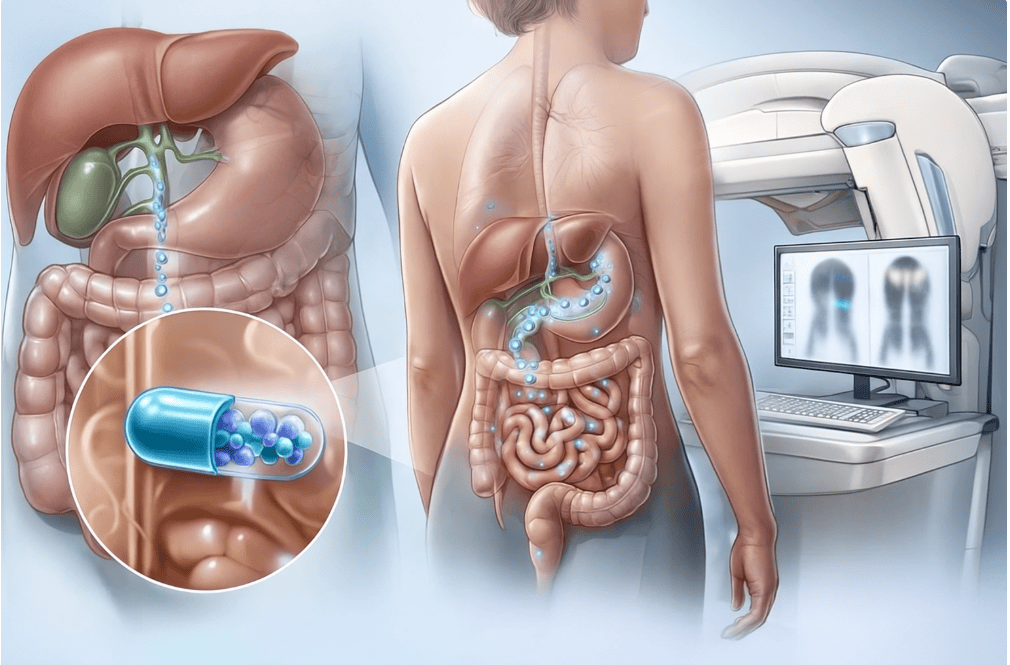
The SeHCAT (7α-[75Se]-taurocholic acid) test is a functional nuclear medicine method used to quantify enterohepatic recirculation of bile acids and diagnose bile acid malabsorption (BAM).
The patient orally ingests a capsule containing a radioactively labelled bile acid analogue (^75Se-homotaurocholate). This substance is absorbed in the small intestine, passes into the portal circulation and is re-excreted into the bile in the liver – just like endogenous bile acids. The amount of radioactivity retained in the body after a certain period of time (usually after 7 days) corresponds to the efficiency of the enterohepatic cycle.
The method uses a planar gamma camera and simple multiple retention measurements – after swallowing the capsule, the first scintigraphy is performed (day 0), followed by a control measurement after 7 days. The ratio of activity on day 7 to activity on day 1 expresses SeHCAT retention (%).
Main clinical indications
- Chronic watery diarrhoea of unclear aetiology – differentiation between irritable bowel syndrome (IBS-D) and BAM.
- Post-cholecystectomy syndrome – assessment of excessive loss of bile acids into the colon.
- Ileal resection or terminal ileum involvement (Crohn's disease) – impaired reabsorption of bile acids.
- Radiation enteritis – loss of functional absorption capacity of the ileum.
- Postoperative or idiopathic malabsorption of bile acids.
- Monitoring the efficacy of treatment with bile acid sequestrants (cholestyramine, colesevelam).
Contraindications and patient preparation
- Absolute contraindications: pregnancy.
- Relative: breastfeeding (must be discontinued for 24 hours), severe swallowing disorders.
- Patient preparation:
- no special dietary restrictions, light meals are recommended,
- the patient should discontinue bile acid sequestrants 7 days prior to the examination,
- no need to discontinue regular medication.
The examination is completely non-invasive and very well tolerated.
Examination procedure
- Day 0:
- The patient takes a capsule containing 75Se-SeHCAT (activity usually 370 kBq) orally.
- after 3 hours, the first scintigraphic measurement is performed (whole-body anterior and posterior images, or regional images of the abdomen).
- Day 7:
- repeated measurement in the same projection and position,
- evaluation of the ratio of retained activity (day 7 vs. day 0).
- Result:
- SeHCAT retention [%] = (activity on day 7 / activity on day 0) × 100.
Interpretation and clinical significance
- Normal retention: > 15% (in some protocols > 10%).
- Slightly reduced (borderline) retention: 10–15%.
- Pathological retention: < 10% – confirms the diagnosis of bile acid malabsorption (BAM).
- Severe form: < 5% – typical for terminal ileal involvement or extensive resections.
Reduced SeHCAT retention indicates loss of effective enterohepatic circulation – bile acids escape into the colon, where they stimulate the secretion of water and electrolytes and cause secretory diarrhoea.
The result has significant therapeutic implications, as it allows for the targeted initiation of treatment with bile acid sequestrants and the differentiation of patients from those with IBS-D, who have a different pathophysiology.
Advantages and limitations
Advantages:
- High sensitivity and specificity (~90–95%).
- Low radiation exposure (~0.25 mSv).
- Simple, non-invasive and reproducible examination.
- Possibility of quantitative evaluation and monitoring of treatment response.
Summary for practice
The SeHCAT examination is:
- the gold standard for the diagnosis of bile acid malabsorption (BAM),
- key to the differential diagnosis of chronic diarrhoea,
- non-invasive, safe and quantitative,
- significantly helps to indicate the correct therapy with bile acid sequestrants.
When correctly indicated and interpreted, the SeHCAT test is an irreplaceable tool in gastroenterological practice, enabling accurate diagnosis of enterohepatic circulation disorders and thus significantly improving the quality of life of patients with chronic diarrhoea.