Perfusion scintigraphy of the lungs
A practical guide for referring physicians
Principle and method
Lung perfusion scintigraphy is an established method in nuclear medicine that allows regional lung perfusion to be visualised and is an indispensable tool in the diagnosis of a number of lung diseases.
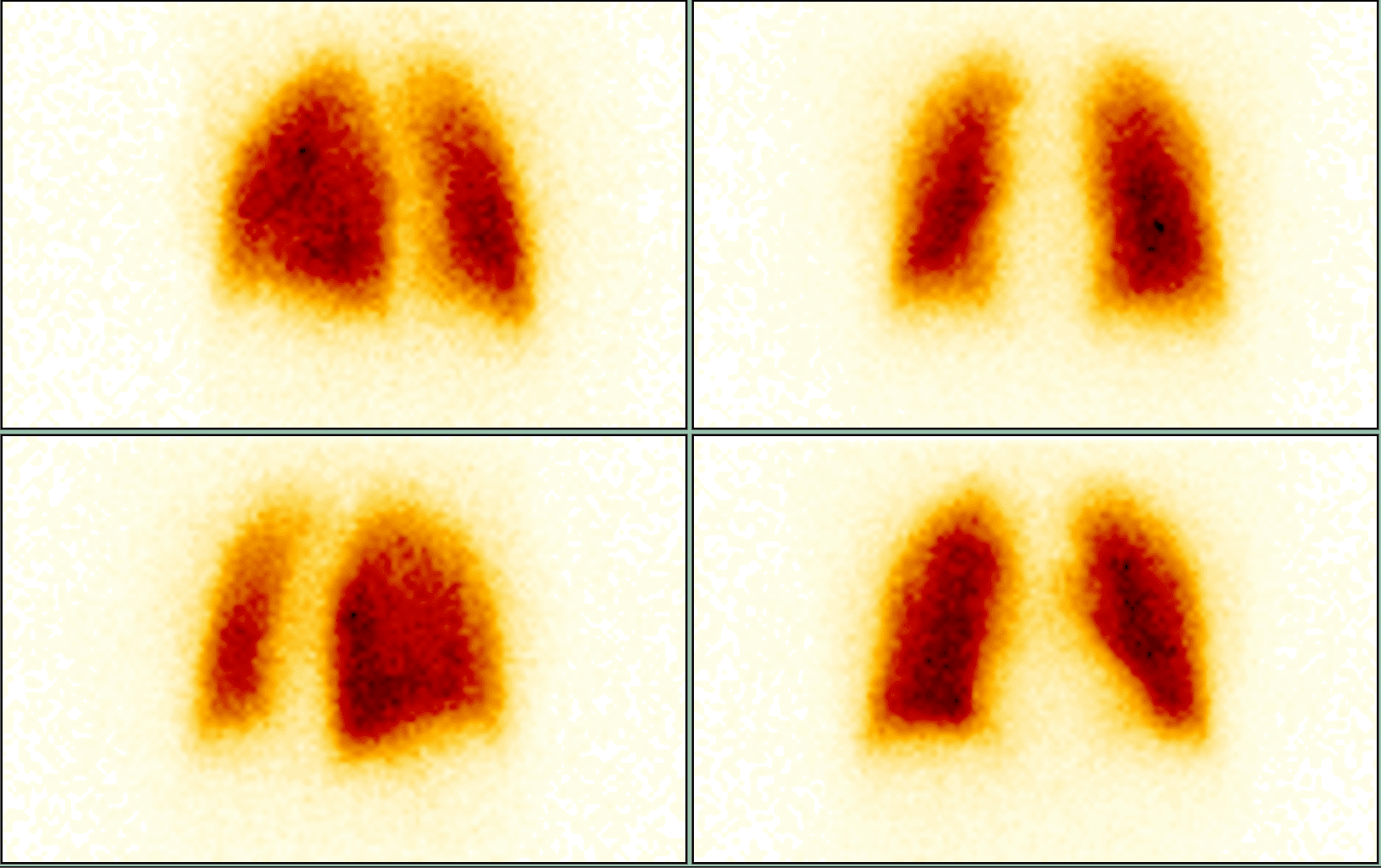
After intravenous administration of 99mTc-albumin macroaggregate (MAA), microembolisation occurs in the pulmonary capillaries. The distribution of the radiopharmaceutical corresponds to the regional blood flow in the pulmonary circulation. Scintigraphy thus allows functional and quantitative assessment of the perfusion of both lungs and individual lung lobes.
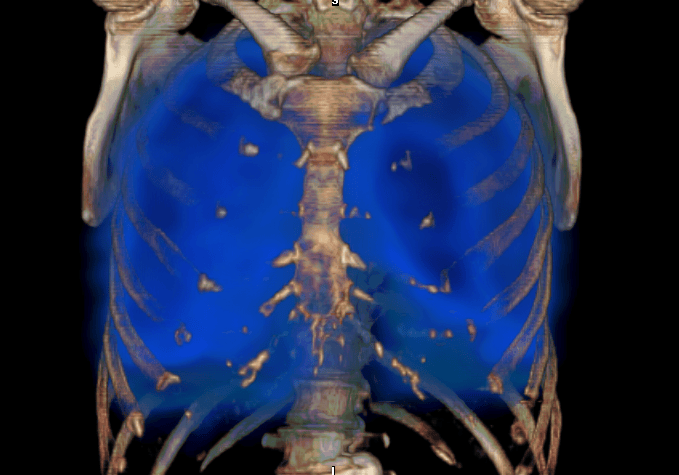
The examination is routinely performed in a planar manner in several projections and, in indicated cases, also using SPECT or SPECT/CT, which increases specificity and facilitates interpretation.
Main clinical indications
1. Pulmonary embolism (PE)
- The basic and historically best-known indication.
- Principle: perfusion defects in PE are characteristically mismatched (they do not correlate with ventilation in a combined V/Q examination).
- The method has high sensitivity and, in combination with ventilation, is still recommended in European and American guidelines as a standard alternative to CT pulmonary angiography (CTPA), especially in patients with contraindications to CT (contrast agent allergy, renal insufficiency, pregnancy).
2. Preoperative examination in thoracic surgery
- Quantification of regional perfusion prior to planned lung resection (lobectomy, pneumonectomy).
- Enables prediction of postoperative function and risk of respiratory insufficiency.
3. Chronic thromboembolic pulmonary hypertension (CTEPH)
- Perfusion scintigraphy is highly sensitive in detecting chronic perfusion defects.
- It is used for early diagnosis and monitoring of patients indicated for surgical endarterectomy or pharmacological treatment.
4. Other indications
- Assessment of the functional significance of unilateral pulmonary lesions (tumours, atelectasis, fibrosis).
- Examination as part of lung transplant evaluation (donor vs. recipient).
- Functional supplement to HRCT and MRI in interstitial and vascular lung diseases.
Interpretation
Positive findings
- Perfusion defects localised segmentally or subsegmentally, sharp borders → suspected pulmonary embolism.
- Inhomogeneous perfusion → chronic thromboembolic pulmonary hypertension.
- Decreased or absent perfusion throughout the lobe/lung → corresponds to obstruction of large vessels, tumour or postoperative condition.
Practical information for the referring physician
- Patient preparation: none; fasting is not necessary.
- Radiopharmaceutical: 99mTc-MAA, intravenous administration, dose according to age and weight.
- Examination procedure:
- i.v. administration of radiopharmaceutical in a supine position (minimisation of particle sedimentation),
- imaging in several projections (usually 6–8),
- SPECT/CT supplementation in indicated cases.
- Examination duration: max. 20 minutes
- Radiation exposure: low, approx. 1.5–2.5 mSv.
- Contraindications: pregnancy (relative); caution in severe pulmonary hypertension (risk of microembolisation when administering a large number of particles).
Clinical examples
- Patient with shortness of breath and contraindication to contrast agent – perfusion scintigraphy shows multiple segmental defects → diagnosis of pulmonary embolism confirmed, anticoagulation therapy initiated.
- Male patient with lung cancer scheduled for pneumonectomy – perfusion quantification shows dominant function of the contralateral lung, surgical procedure can be performed safely.
- Patient with suspected CTEPH – perfusion scan reveals chronic perfusion defects in the lower lobes → diagnosis confirmed and endarterectomy indicated.
Summary for practice
Lung perfusion scintigraphy is:
- a highly sensitive method for detecting acute and chronic pulmonary embolism,
- indispensable in preoperative evaluation and diagnosis of CTEPH,
- safe and low in radiation exposure, suitable even for patients with contraindications to CT angiography,
- in combination with ventilation scintigraphy (V/Q scan), it provides the highest diagnostic accuracy.
Although it is being replaced by CT techniques in some cases, it continues to have a firm place in the diagnosis of pulmonary embolism and other lung diseases and is a key tool in the care of patients with shortness of breath and respiratory failure. It has a lower radiation exposure and does not use contrast agents.