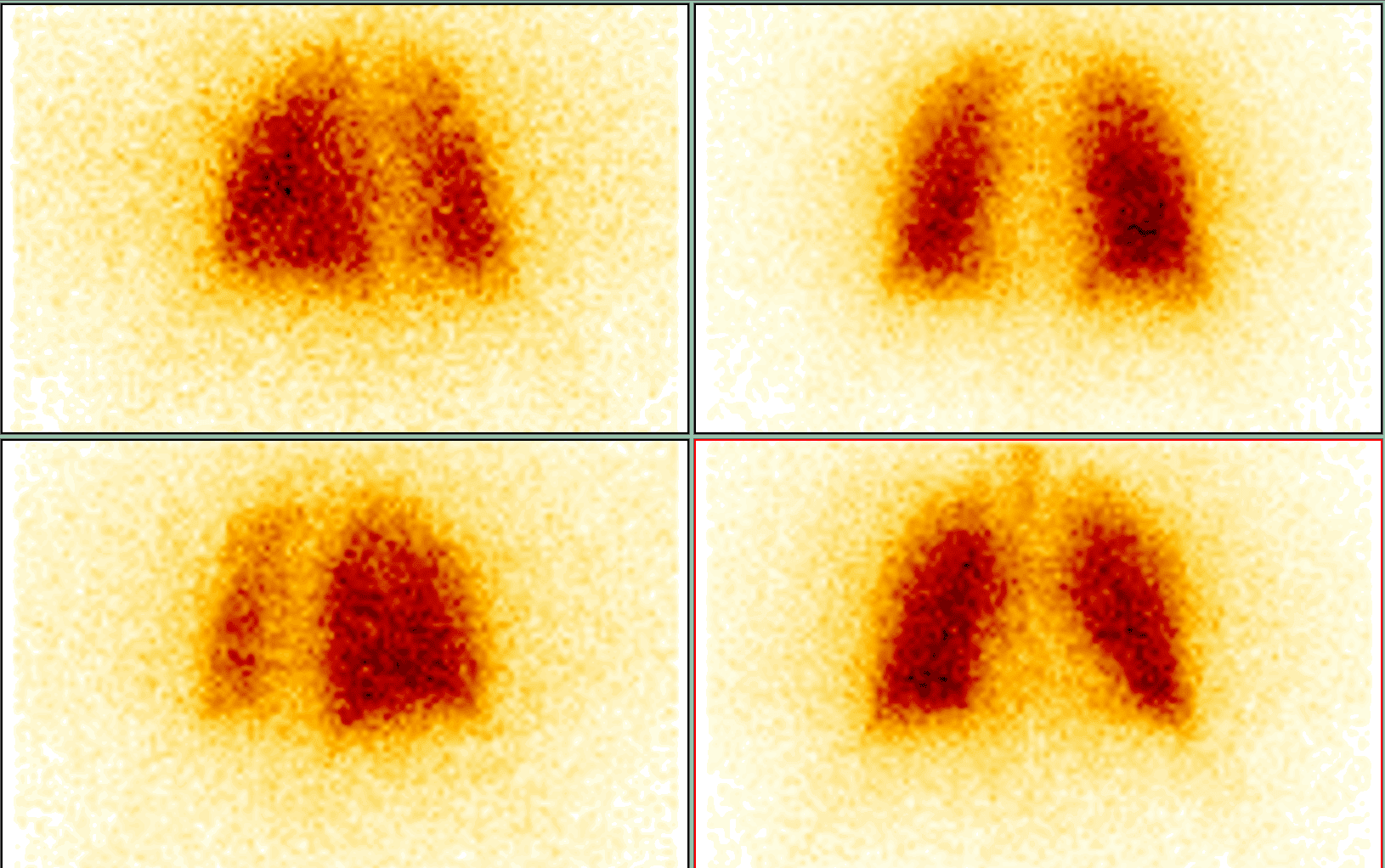
Ventilation scintigraphy of the lungs
A practical guide for referring physicians
Principle and method
Ventilation scintigraphy of the lungs is a functional radionuclide method that allows regional lung ventilation to be visualised and correlated with perfusion. Its main benefit lies in its combination with perfusion scintigraphy (known as a V/Q scan), which provides essential information about the ventilation/perfusion ratio and is the basic method for diagnosing pulmonary embolism (PE).
Radiopharmaceuticals used for ventilation studies:
- 81mKr (krypton) – an inert gas, ideal for continuous inhalation, has a short half-life (13 s) but limited availability.
Imaging is performed planarly in several projections, but increasingly using SPECT/CT, which allows three-dimensional evaluation and fusion with CT images.
Main clinical indications
1. Diagnosis of pulmonary embolism (PE)
- In combination with perfusion scintigraphy, ventilation scanning is a standard and validated method for detecting PE.
- A mismatch of perfusion defect (normal ventilation but impaired perfusion) is a typical picture of acute embolisation.
- Conversely, matched defects (impaired ventilation and perfusion) are more indicative of other pulmonary pathologies (e.g. COPD, pneumonia, tumour).
2. Preoperative examination in thoracic surgery
- Quantification of regional ventilation before planned resection (lobectomy, pneumonectomy).
- Enables prediction of postoperative function and risk of respiratory insufficiency.
3. Chronic obstructive pulmonary disease (COPD) and asthma
- Evaluation of ventilation distribution, assessment of the degree and distribution of ventilation disorders.
- Use in differential diagnosis to distinguish between restrictive and obstructive disorders.
4. Interstitial and other lung diseases
- Ventilation scintigraphy can document irregularities and provide a supplement to HRCT or MRI.
5. Transplant medicine
- Assessment of regional lung function in donors and recipients, monitoring of graft function.
Interpretation
Positive findings
- Mismatch – preserved ventilation, impaired perfusion → typical for PE.
- Matched defect – ventilation and perfusion reduced to the same extent → chronic or structural lung disease.
- Diffuse ventilation disorders – typical in COPD, emphysema or severe asthma.
Practical information for the referring physician
- Patient preparation: no preparation required; the patient must be able to cooperate during inhalation.
- Examination procedure:
- inhalation of radiopharmaceutical (gas or aerosol),
- imaging in several projections (planar or SPECT/CT),
- followed by perfusion scintigraphy for correlation.
- Examination duration: 20–40 minutes (ventilation + perfusion).
- Radiation exposure: very low (ventilation component approx. 0.2–1 mSv, total V/Q examination 1.5–3 mSv).
- Contraindications: relative – patients unable to cooperate during inhalation.
Summary for practice
Ventilation scintigraphy of the lungs is:
- a key method in combination with perfusion scintigraphy for the diagnosis of PE,
- essential in planning lung surgery,
- valuable in the evaluation of ventilation disorders in COPD, asthma and interstitial diseases,
- safe, with minimal radiation exposure and a wide range of clinical indications.
Together with the perfusion part (V/Q scan), it is one of the most sensitive methods for detecting pulmonary embolism and significantly complements modern imaging algorithms.